COMPLEX MANAGEMENT OF AN ADVANCED CAESAREAN
SCAR PREGNANCY (CSP) – CASE REPORT AND SHORT
REVIEW OF LITERATURE
Marina Dinu, Roxana Drăguşin , Ştefania Tudorache,
Maria Şorop-Florea, C.L. Pătru , D. Iliescu
* Emergency University Hospital Craiova, Romania
** University of Medicine and Pharmacy, Craiova, Romania
Abstract
Cesarean scar pregnancy (CSP) is a rare medical condition with an increased incidence due to a high
number of Cesarean deliveries. There are several management options including a conservative approach by
administration of systemic and /or local Methotrexate (Mtx) as well as bilateral uterine artery embolization (UAE)
and dilatation and curettage. We, hereby, present the case of a patient diagnosed with a viable CSP. UAE was
proposed to reduce the hemorrhagic complications before and during dilatation and curettage. We would like to
underline that CSP requires early diagnosis and appropriate management to avoid severe complications in patients
who want to maintain fertility. Although there is little data on this pathology, conservative treatment can be an
optimal treatment even in the presence of fetal heart activity, or in the presence of a the large gestational sac.
Introduction
Caesarean scar pregnancy (CSP) is considered a rare and life-threatening type of ectopicpregnancy. The first case of CSP was reported in 1978 (1). Nowadays, the rate of CSP is 1 in 2000 cases and accounts for 6% all ectopic pregnancies among women with a prior caesarean delivery (2). As the rate of caesarean delivery is increasing worldwide, the CSP pathology will likely become a very frequent entity in the near future. Fortunately, its detection is improving through the widespread use of transvaginal ultrasound (3) and magnetic resonance imaging may add valuable information in selected
Complex management of an advanced caesarean scar pregnancy (CSP) – case report and short review of literature cases, especially when potentially severe complications are suspected (10). All this imagistic information concurs for the success of conservative
(non-surgical) management. Multiple therapeutic options have been proposed as treatment strategies, with no specific consensus established, largely due to its rarity and small samples sizes. Various methods were used, as the dilatation and curettage, excision of trophoblastic tissues using laparotomy or laparoscopy, local and/or systemic Methotrexate (MTX) administration, bilateral hypogastric artery ligation under laparoscopic guidance associated with dilatation and evacuation, and selective uterine artery embolization (UAE) in association with curettage and/or MTX injections; nonetheless, the most appropriate one has yet to be clearly determined (20,21). Overall, CSP is considered a distinct entity when compared with other types of ectopic pregnancies as it is never diagnosed in the first pregnancy and will never occur in women with no history of caesarean delivery. We report a case of a CSP with a live embryo that was treated using MTX systemically and locally associated with bilateral embolization of uterine arteries.
Case Report
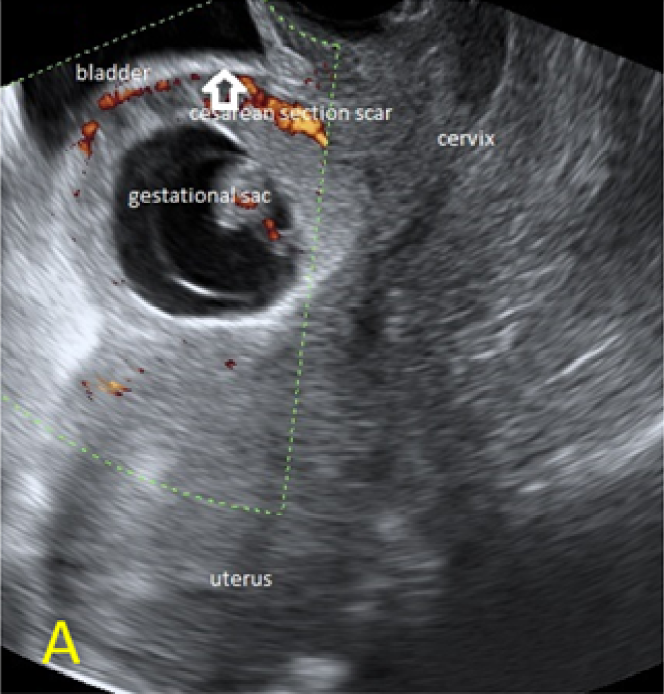
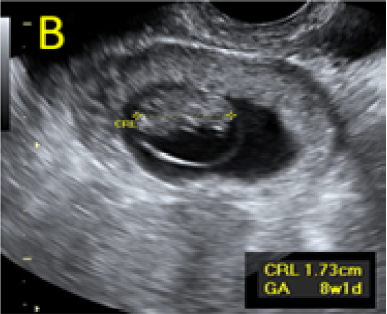
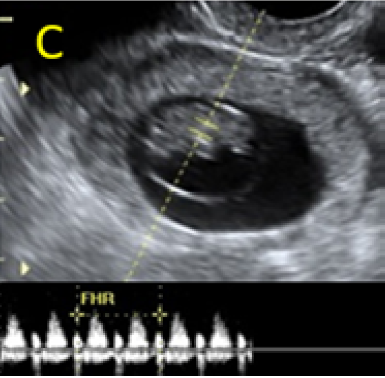
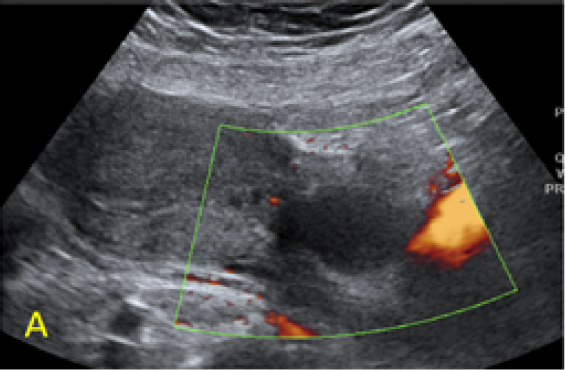
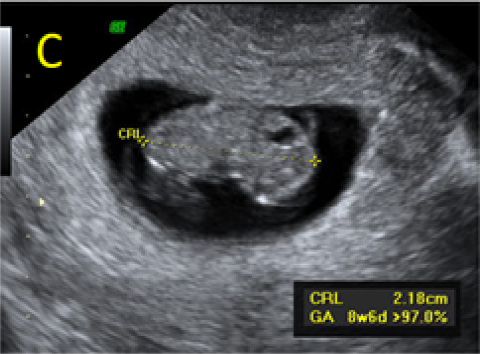
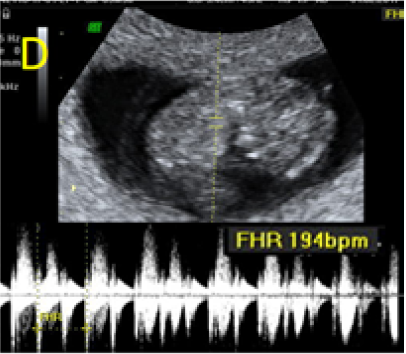
A 22-year-old secundigravida, presented to our Hospital with acute pelvic pain and vaginal bleeding. Her medical history included a 2-year prior caesarean delivery. The patient was in a stable condition and the clinical exam was unremarkable. As the urinary pregnancy test was positive, a transvaginal ultrasound scan was performed to evaluate the pregnancy location and viability. The exam revealed an empty uterine cavity but identified the gestational sac at the level of the caesarean scar with a live embryo (174 beats per minute), measuring 8 weeks and 5 days by crown-rump length. (Figures 1). Because the trophoblastic tissue was noted with an anteriorly location, urinary bladder invasion was suspected based on the ultrasonographic signs: poor identification of the bladder wall, the lack of the sonolucent space and increased vascularization with abnormal pattern (Figure 2). The patient blood tests results were normal, and beta-human chorionic gonadotropin (b-HCG) value was 145.000mUI/ml. After proper counselling and written informed consent the patient opted for a medical conservative treatment with desire to preserve her fertility.
Figure 1. A: the gestational sac is located at the level of the uterine isthmic scar, grey-scale and Power Doppler transvaginal evaluation. B: an embryo with a crown-rump length (CRL) that corresponds to 8 weeks and 1 day is found with normal fetal heart activity (C).
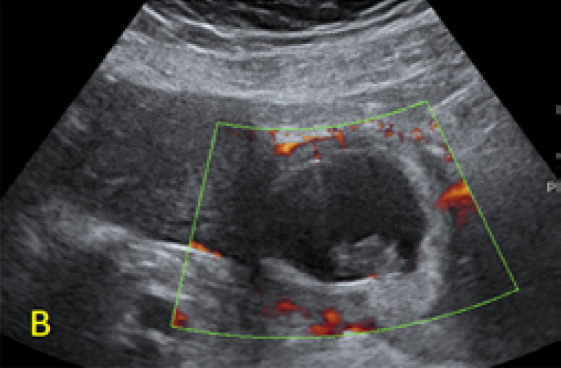
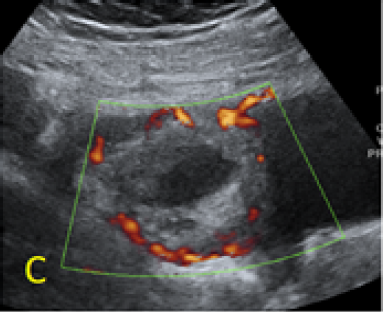
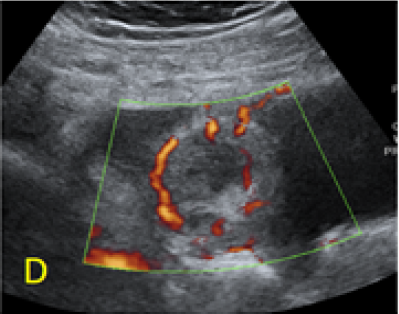
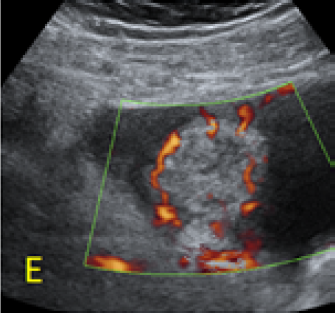
Figure 2. A, B: empty uterine corpus and the presence of the gestational sac at the level of the previous cesarean scar, transabdominal assessment. C, D, E: Same approach, evidence of bulging of the gestational sac into the urinary bladder, with hypervascularity highlighted using Power Doppler evaluation.
Figure 3 – Ultrasound evaluations on Day 3 (A, B) and 7 (C, D) after MTX administration, with B-hCG values of 103.016 and 57.710mUI/ml, respectively. Fetal growth and normal heart activity is present.
Because of the high gestational age, β-hCG level and alarming ultrasound appearance, a conservatory but complex management was decided. The patient received a systemic single dose regimen of Methotrexate (MTX) of 90 mg administered intramuscularly (50mg/m2), followed by bilateral uterine artery embolization (UAE) with Gelaspon embospheres.
According to the hospital protocol, â-hCG was dosed on day 4 after administration with a
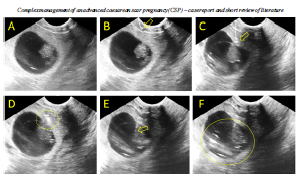
Figure 4. Local administration of MTX procedure. The aspect before injection (A), insertion of the needle in the uterine wall (B) and the trophoblast (C). Injection of the MTX in the trophoblastic area (D) and progression of the needle in the embryonic area of the gestational sac (E) with the administration of the rest of the dose (F) reported value of 103.016mUI/ml. Ultrasound
assessment revealed the persistence of embryonic cardiac activity and intense trophoblastic vascularization. HCG constantly decreased to 57,710mUI/ml on day 7 after MTX administration but the embryonic cardiac activity was still noted with a normal rate.
We considered that the initial protocol failed to fulfill its purposes, and because of an imminent severe complication, we decided further active management. Using transabdominal ultrasound guidance, with a thin 22-Gauge needle, 25 mg of MTX ware injected transvaginally in the gestational sac, in the embryonic area and another 25mg of were injected in the trophoblastic tissue (Figure 4). To reduce the patient’s discomfort and anxiety, local methotrexate injection under transvaginal ultrasound guidance was performed under general anesthesia with the patient in the lithotomy position. 24 hours later the scan confirmed that the fetal cardiac activity ceased.
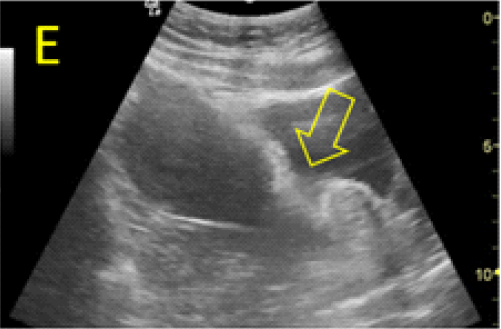
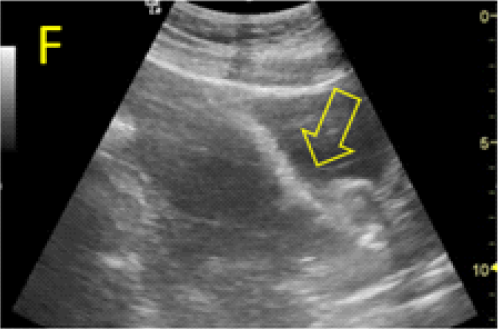
Dilatation and curettage (D&C) under ultrasound guidance was proposed for a safe, precise and rapid evacuation of the gestational sac. In order to further avoid bleeding complications, angiographic investigation of the pregnancy site was re-scheduled and performed 24 hours prior to the surgical evacuation of the CSP, due to the potential degradation of the embolic material and secondary revascularization. Indeed, a significant flow was identified, and bilateral re-embolization was performed. The cervical dilation and pregnancy aspiration were performed under sonographic guidance (Figure 5, A-D). In our opinion, the careful and complex management was very important, as the bladder-uterine interface appeared severely damaged, with the easily translation of the bladder wall inside the isthmic uterine segment through the scar area when the pregnancy war evacuated by aspiration (Figure 5, E-F).
The following day the surgical procedure, β-hCG dropped to 9770mUI/ml and subsequently was
dosed weekly, until the level was negative, one month later. Almost one year later, the patient presented with
a normally located and viable pregnancy.
Discussion
Even with the rapid increase in the incidence of CSP, this type of pregnancy remains the rarest form of ectopic pregnancy (2). Most of CSP cases are reported in the first trimester (4). Firstly, we must underline that early diagnosis is essential for an effective non-surgical management, and also reducing morbidity and fatal complications. Today, transvaginal color flow Doppler examination is easy accessible and highly accurate in the differential diagnosis of CSP and also for an adequate follow-up (5).
Figure 5. Cervical dilation and pregnancy aspiration performed under transabdominal sonographic guidance. A: the appearance before the procedure, the gestational sac bulging in the urinary bladder is marked with open star. B:Cervical dilation, the metallic Hegar dilator is indicated with open arrow. C, D: progressive aspiration of the pregnancy. E, F: translation of the posterior bladder aspect (open arrow) inside the isthmic uterine segment, through the pregnancy scar area, at the time of aspiration.
The main aim of treatment for CSP is to prevent massive blood loss and preservation of uterus to maintain future fertility (6). Multiple treatments have been proposed as CSP is considered to have an aggressive behavior with a high risk for uterine rupture and bleeding, endangering future fertility (8). Still there is no consensus on the best approach of CSP. Management plans were proposed based on the gestational age, HCG levels and presence of a viable pregnancy or not. In the past, the favorite CSP management was the operative intervention including dilatation and curettage (8), or excision of the trophoblastic tissue using either laparotomy (5) or laparoscopy (9).
In 2004, Maymon et al. (10) suggested emergency laparotomy and excision of the cesarean scar pregnancy site as an effective management, in 15 reported cases. In 2006, Lee et al. (11) reported the excision of CSP by laparoscopic surgery and by now, 49 cases have been described, with a complication rate of 30%. In 2005, Wang et al. (12) described a successful CSP treatment by operative hysteroscopy and suction curettage, with a short operative time (mean 36.7 ± 20.8 minutes), less blood loss (mean 50.0 ± 0.0 ml), short postoperative stay (mean 1.1 ±0.9 days) and a rapid return of the pregnancy test to negative (<4 weeks, mean 22 days) (13). Still, due to a high rate of bleeding complications, these therapeutic methods have been left as an ultimate solution, while a more conservative approach was preferred especially in young, stable patients.
MTX used systemically or locally is considered the first line of a conservative approach of CSP (14) since it was introduced in the 90’s (4, 15,16). The systemic regimen of MTX may include repeated doses due to its short half-life (10 hours) and also because the fibrous tissue of the scar may decrease the absorption of the drug (15). On the other hand, the local regimen of MTX achieves higher drug concentrations avoiding the systemic side effects. More, the intralesional injection proved to be more effective in cases where the HCG is more than 5000 mUI/ml (2) and also patients with a relatively large gestational sac (> 5 cm in diameter) or type II CSP much more likely to have an unsuccessful outcome (17). UAE was introduced in the 90’s as a conservative treatment for medical conditions with important bleeding risk such as postpartum hemorrhage, uterine myoma and ectopic pregnancy (18, 19) or as a prevention massive bleeding method during surgical procedures (20). Recently, direct administration of MTX to the gestational mass after bilateral UAE has proved to be an effective conservative management strategy for patients with CSP (17). Sugawara et al. (21) reported 3 cases of CSP that were successfully managed by UAE and direct injection of MTX to the gestational mass and surrounding myometrium; systemic MTX was also administered when â-hCG normalization was not satisfied (22). Hasegawa et al. suggested that surgical repair of the scar as either the initial management or secondary after the MTX treatment, might be a preferable option for patients who wish to preserve fertility in the future (23).
In our case, given the high-risk related to the increased gestational age, we considered dilatation and curettage only after previous conservative complex management, to minimize the bleeding complications risk, as previously proven (24,25).
Other treatment options include hysteroscopy with coagulation of the blood vessels at the implantation site, laparoscopy or laparotomy in hemodynamically unstable patients and transvaginal hysterotomy (26). The surgical treatment including D&C has the main advantage to remove the gestational sac with a rapid decrease of HCG, still the uterine integrity cannot be guaranteed (27). In our case, the value of HCG returned to normal in 1 month.
Due to the clinical lack of response and the unsatisfactory decrease of HCG value after the first
MTX & UAE association, we continued the conservatory management, by adding a local dose regimen of MTX on day 7. Still, we proposed reembolization before dilatation and curettage to ensure the least complications and the best chances to preserve fertility. The rationale for repeating the procedure was the time interval passed from the initial UAE, that permitted uterine re-vascularization, and the Doppler appearance of a significant peritrophoblastic flow.
As there are no reports of the teratogenic risks for a new pregnancy following the use of MTX (27), our patient was counselled to avoid a new pregnancy for at least 3 months. A new viable intrauterine pregnancy was obtained in less than 1 year with no major difficulties or complications. Nevertheless, future pregnancy and prevention of recurrence are the first priority to consider in the management of recurrent CSP. The present literature reports only 3 cases of recurrent CSP (15), however a new pregnancy in a patient with a CSP history must benefit by special attention regarding its location, placentation and uterine scar later compliance.
As a small case series, in our Clinic, between 2013 and 2016, 8 women were referred with a
suspicion of CSP. All cases had detailed ultrasonographic (US) assessment and serial measurements of HCG. All patients were counseled regarding the benefits and potential risks of the MTX treatment and written informed consents were obtained.
One patient opted for preservation of the pregnancy, despite all the hemorrhagic risks, and she delivered a viable fetus followed by an emergency hysterectomy. 5 patients received a single dose regimen of MTX (1mg/kgc) in combination with UAE and followed by a US guided D&C without any other incidents. In one case, UAE followed by and D&C proved to be successful. In one case MTX, UAE and D&C resulted in emergency hysterectomy due to important blood loss. The histopathological diagnosis described coriocarcinoma. In the past, between 2010 and 2013, in our Clinic were registered 6 patients treated by D&C and 4 four of which required an immediate hysterectomy.
Conclusion
Prompt diagnosis and treatment of CSP are essential in patients who want to preserve their fertility. Although there are no specific guidelines on the optimal treatment of an advanced CSP, in stable patients a combination of the conservative methods
is recommended. Professionals should consider changing the conservative approach when the initial protocol fails and the association of UAE for an optimal management to avoid complications before dilatation and curettage.
As there are no evidence-based recommendations available, clinicians depend on the available case reports regarding various treatment options.